
Allevi Blog
Allevi Author – Valentine’s Edition: 3D Bioprinting Aortic Valves
- Updated on April 13, 2020
On this very special Valentine’s Day edition of #AlleviAuthor, we’d like to introduce our newest member of the #alleviauthor club whose work studies bioprinting to repair broken heart…valves. Benjamin Stewart, whose thesis was recently presented to the faculty of the Daniel Felix Ritchie School of Engineering and Computer Science at the University of Denver, studies cardiac tissue specifically for aortic valve repair. He has been exploring new methods for 3d bioprinting aortic valves in his newly published paper.
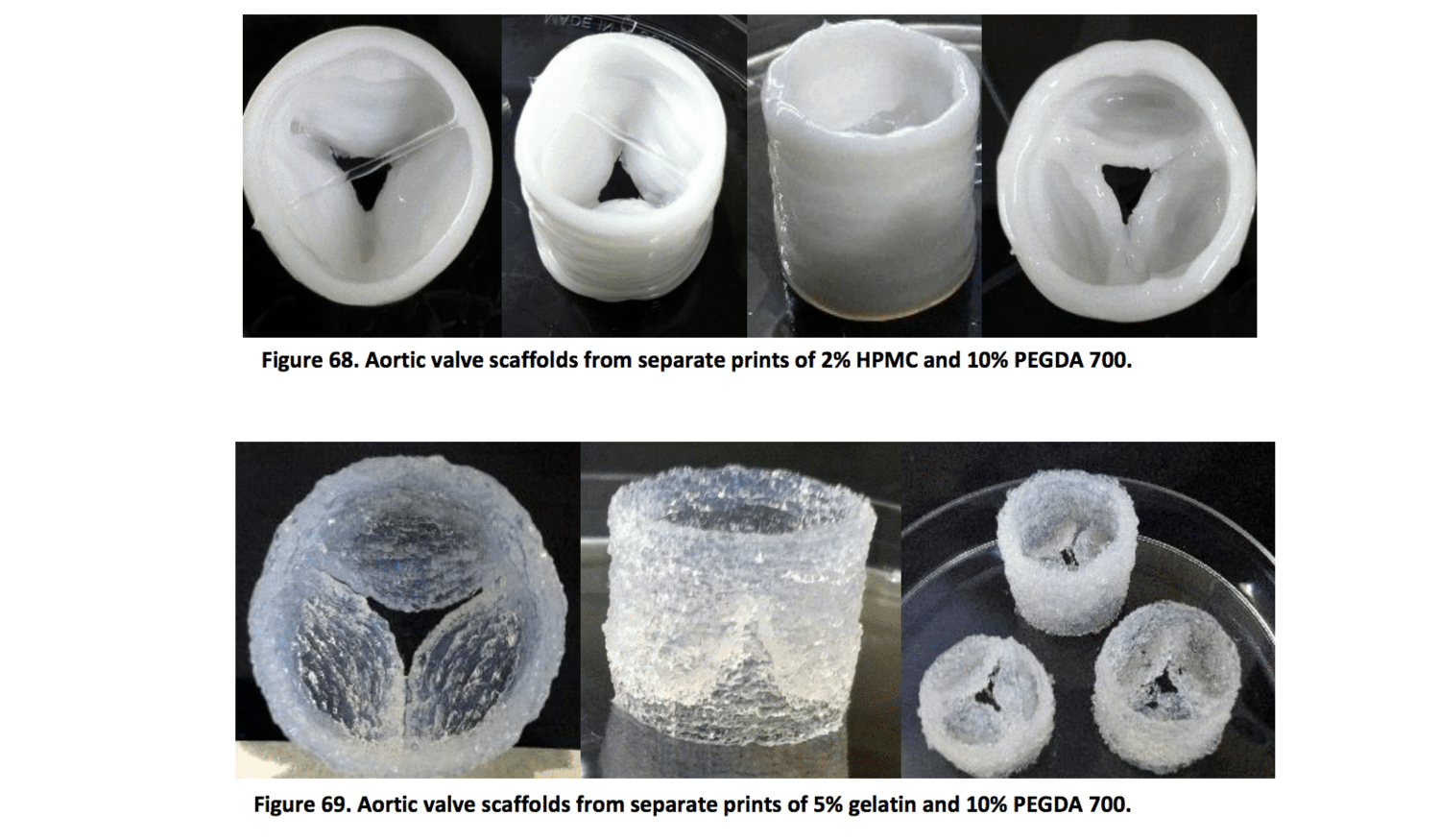
Stewart’s work focuses on 3D bioprinting hydrogels for tissue-engineered ascending aorta scaffolds using the AlleviBeta 3D bioprinter. Biocompatible polymers were tested for extrusion mechanics, mechanical and fluid properties, crosslinking dynamics, and degradation properties. Mechanical stretch properties and dynamic performance were tested extensively.
One of the most important aspects of 3D bioprinting is finding the correct biocompatible materials that mimic the mechanical properties of the tissues in your body. Stewart’s extensive materials research lays the groundwork for future bioink development for cardiac clinical applications. With the correct bioink, doctors could one-day bioprint replacement parts that mechanically perform just like the healthy cardiac tissue in your body. Read on to learn more.
ABSTRACT: The gold standard in 2016 for thoracic aortic grafts is Dacron®, polyethylene terephthalate, due to the durability over time, the low immune response elicited and the propensity for endothelialization of the graft lumen over time. These synthetic grafts provide reliable materials that show remarkable long term patency. Despite the acceptable performance of Dacron® grafts, it is noted that autographs still outperform other types of vascular grafts when available due to the recognition of the host’s cells and adaptive mechanical properties of a living graft. 3D bioprinting patient-specific scaffolds for tissue engineering brings the benefits of non-degrading synthetic grafts and autologous grafts together by constructing a synthetic scaffold that supports cell infiltration, adhesion, and development in order to promote the cells to build the native extracellular matrix in response to biochemical and physical cues.
Using the Allevi 3D bioprinter, scaffold materials we tested non-Newtonian photosensitive hydrogel that formed a crosslinked matrix under 365 nm UV light with appropriate water content and mechanical properties for cell infiltration and adhesion to the bioprinted scaffold. Viscometry data on the PEGDA-HPMC 15%-2% w/v hydrogel (non-Newtonian behavior) informed CFD simulation of the extrusion system in order to exact the pressure-flow rate relationship for every hydrogel and geometry combination. Surface tension data and mechanical properties were obtained from material testing and provide content to further characterize each hydrogel and resulting crosslinked scaffold. The goal of this work was to create a basis to build a database of hydrogels with corresponding print settings and resulting mechanical properties.

